Kawasaki Disease
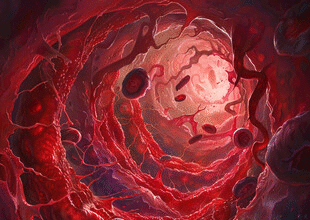
Kawasaki disease (KD) is an acute, self‑limited, medium‑vessel vasculitis of childhood that predominantly affects coronary arteries and can lead to aneurysm formation without early treatment. It is the leading cause of acquired heart disease in children in many developed regions.
- Epidemiology
- Etiology & Pathogenesis (Brief)
- Classic (Complete) Diagnostic Criteria
- Incomplete (Atypical) Kawasaki Disease
- Additional Clinical/Lab Findings
- Differential Diagnosis
- Cardiac Complications
- Initial Treatment (Within 10 Days of Fever Onset)
- IVIG Resistance (Persistent/Recurrent Fever ≥36 h After Completion)
- Antithrombotic Strategy by Coronary Status
- Echocardiography Follow-Up (Typical)
- Long-Term Management
- Prognosis
- When to Suspect / Refer Urgently
- Key Takeaways
Epidemiology
- Age: majority <5 years; peak 9–24 months.
- Sex: slight male predominance.
- Higher incidence in East Asian populations globally (genetic susceptibility + triggers).
- Seasonal clustering (late winter–spring) and occasional community outbreaks suggest environmental/infectious triggers.
Etiology & Pathogenesis (Brief)
Exact trigger unknown; likely an abnormal immune response to one or more ubiquitous agents in genetically predisposed children. Immune activation leads to systemic inflammation, endothelial injury, and panvasculitis of medium arteries with a predilection for coronaries.
Classic (Complete) Diagnostic Criteria
Fever ≥5 days (often high, unresponsive to antipyretics) PLUS ≥4 of 5 principal features (can diagnose earlier if criteria met and coronary changes present):
- Bilateral, non‑exudative conjunctival injection (limbal sparing).
- Oral mucosal changes: erythema, fissured lips, “strawberry” tongue, diffuse oropharyngeal injection.
- Polymorphous rash (maculopapular, morbilliform, erythema multiforme–like; not vesicular/bullous).
- Extremity changes: acute phase—erythema/edema palms and soles; convalescent—periungual desquamation (weeks 2–3).
- Cervical lymphadenopathy (≥1 node ≥1.5 cm), typically unilateral.
Coronary artery involvement may appear on echocardiography (dilatation or aneurysms) and supports diagnosis even if fewer criteria present.
Incomplete (Atypical) Kawasaki Disease
Consider when fever ≥5 days with 2–3 principal features, especially in infants <6 months (may present with prolonged fever and elevated inflammatory markers). Laboratory clues: elevated CRP/ESR, leukocytosis with neutrophilia, anemia, thrombocytosis (after day 7), hypoalbuminemia, elevated ALT, sterile pyuria.
Algorithm: If CRP ≥3 mg/dL or ESR ≥40 mm/h and supportive lab abnormalities (≥3 among anemia, thrombocytosis after day 7, ALT elevation, hypoalbuminemia, WBC ≥15K, sterile pyuria), obtain echocardiogram; treat if echocardiogram abnormal or persistent systemic inflammation.
Additional Clinical/Lab Findings
- Irritability (common, sometimes severe).
- Myocarditis, pericardial effusion, valvulitis (mitral regurgitation) early.
- Thrombocytosis peaks weeks 2–3 (>450K/µL).
- Elevated BNP/NT‑proBNP may reflect myocardial strain.
Differential Diagnosis
Measles, adenovirus, scarlet fever, toxic shock syndrome, Stevens–Johnson syndrome, multisystem inflammatory syndrome in children (MIS-C), juvenile idiopathic arthritis, drug reactions.
Cardiac Complications
- Coronary artery ectasia and aneurysms (risk highest without IVIG; reduced from ~25% to <5% with timely therapy).
- Myocarditis, decreased LV function (usually transient).
- Arrhythmias, ischemia, rarely infarction or sudden death in large/giant aneurysms.
Coronary artery dimensions are indexed by Z‑scores (adjusted for body surface area):
| Z-Score | Classification |
|———|—————-|
| <2.0 | Normal |
| 2.0–2.4 | Dilated (prominent) |
| 2.5–4.9 | Small aneurysm |
| 5.0–9.9 | Medium aneurysm |
| ≥10 or diameter ≥8 mm | Giant aneurysm |
Initial Treatment (Within 10 Days of Fever Onset)
- IVIG: 2 g/kg (single infusion over 8–12 h) — administer as soon as diagnosis established (optimal before day 10; still consider later if ongoing inflammation or coronary changes).
- Aspirin: High‑dose (30–50 or up to 80–100 mg/kg/day divided q6h) during acute inflammatory phase until afebrile 48–72 h, then switch to low‑dose (3–5 mg/kg/day once daily) for antiplatelet effect until no coronary changes at 6–8 weeks. (Some centers start with moderate dose; practice varies.)
- Hydration, fever control, monitoring for hemolysis or liver dysfunction if prolonged high‑dose aspirin.
IVIG Resistance (Persistent/Recurrent Fever ≥36 h After Completion)
Options (guided by risk stratification and local protocols):
- Second IVIG dose (2 g/kg).
- Adjunct corticosteroids: e.g., methylprednisolone pulse or prednisolone taper (especially in high-risk patients: very young age, high CRP, early coronary dilation).
- Biologic agents: infliximab (anti‑TNF) single dose; anakinra (IL‑1 blockade) in refractory cases; cyclosporine in select severe recalcitrant cases.
Antithrombotic Strategy by Coronary Status
- No coronary changes: low‑dose aspirin until 6–8 week echocardiogram normal.
- Persistent small aneurysm: continue low‑dose aspirin long term.
- Medium aneurysm: aspirin + consider addition of a second antiplatelet (e.g., clopidogrel) per cardiology.
- Large/giant aneurysm or rapid expansion: anticoagulation (warfarin or low molecular weight heparin) + antiplatelet; monitor for thrombosis.
Echocardiography Follow-Up (Typical)
- At diagnosis (baseline), 1–2 weeks, and 4–6 weeks after onset.
- More frequent imaging (e.g., at 3 months, 6 months, annually) if aneurysms present; advanced imaging (CT angiography, MRI) for large/giant aneurysms or ischemia evaluation.
Long-Term Management
- Risk factor modification (lipids, lifestyle) in those with persistent coronary abnormalities.
- Exercise guidance individualized; severe aneurysms may need activity restriction.
- Vaccination considerations: defer live vaccines ≥11 months after IVIG; ensure influenza vaccination when on chronic aspirin (Reye risk mitigation).
Prognosis
Most children recover fully if treated early. Giant aneurysms carry risk of stenosis, thrombosis, myocardial ischemia; may require interventional cardiology or surgical management later.
When to Suspect / Refer Urgently
- Child with ≥5 days fever plus ≥2 principal clinical features.
- Unexplained prolonged fever in infant <6 months with elevated inflammatory markers.
- Any child with persistent irritability, conjunctival injection, oral changes, extremity swelling, or unexplained cervical lymphadenopathy + systemic inflammation.
Key Takeaways
- Early IVIG (2 g/kg) dramatically reduces coronary aneurysm risk.
- Evaluate atypical/incomplete presentations promptly—especially in infants.
- Use Z‑scores to standardize coronary assessment and guide antithrombotic therapy.
- Persistent or recurrent fever after IVIG merits reassessment and second-line therapy.
Educational information only; clinical decisions should follow current pediatric cardiology and infectious disease guidelines.