Infective Endocarditis (IE)
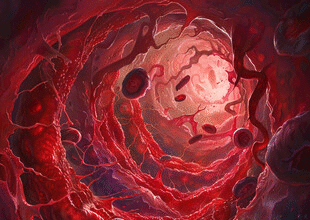
Infective endocarditis is a microbe-driven infection of the endocardial surface (usually cardiac valves, but also septal defects, prosthetic material, endocardial leads). It results from bacteremia or fungemia seeding a thrombotic nidus on damaged endothelium. Despite advances, IE carries high morbidity (embolism, heart failure) and mortality.
- Classification
- Pathogenesis (Simplified Cascade)
- Predisposing Cardiac Conditions
- Non-Cardiac / Procedural Risk Factors
- Microbiology (Evolving Patterns)
- Clinical Manifestations
- Diagnostic Approach
- Empiric Antimicrobial Therapy (Principles)
- Targeted Therapy (Selected Examples)
- Indications for Early Surgical Intervention
- Complications
- Follow-Up & Monitoring
- Prevention (Antibiotic Prophylaxis — Selected Indications)
- Key Takeaways
Classification
- Native valve endocarditis (NVE)
- Prosthetic valve endocarditis (PVE: early <1 year; late ≥1 year after surgery)
- Cardiac device/lead-associated endocarditis
- Right-sided (tricuspid) vs. left-sided (aortic/mitral)
Pathogenesis (Simplified Cascade)
- Endothelial injury (turbulent flow across congenital or acquired lesions, prosthetic material).
- Platelet–fibrin deposition → nonbacterial thrombotic endocarditis (NBTE) nidus.
- Transient bacteremia (dental manipulation, skin infection, invasive procedures, IVDU) seeds nidus.
- Microbial adhesion (adhesins, surface proteins) and proliferation inside protective biofilm + fibrin/platelet matrix.
- Vegetation growth → destruction (regurgitation), embolization, immune phenomena.
Predisposing Cardiac Conditions
- Congenital heart disease (especially unrepaired cyanotic lesions, ventricular septal defect, patent ductus arteriosus, left-sided outflow lesions, bicuspid aortic valve).
- Prosthetic valves, annuloplasty rings, transcatheter valve implants.
- Prior infective endocarditis (strongest risk for recurrence).
- Rheumatic valvular disease, degenerative calcific valve disease.
- Intracardiac devices (pacemaker/ICD leads), vascular access catheters.
Non-Cardiac / Procedural Risk Factors
- Poor dental/oral hygiene, dental procedures with mucosal bleeding.
- Indwelling catheters, hemodialysis.
- Intravenous drug use (right-sided IE, S. aureus predominance).
- Immunosuppression (steroids, biologics), prolonged broad-spectrum antibiotics.
Microbiology (Evolving Patterns)
- Gram-positive cocci dominate: Staphylococcus aureus (now leading in many regions), viridans group streptococci (oral), Streptococcus gallolyticus (bovis group; colonic neoplasia association), enterococci (E. faecalis/faecium—genitourinary or GI source), coagulase-negative staphylococci (prosthetic/device-related).
- HACEK organisms (Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella) — fastidious Gram-negative rods.
- Fungi (Candida, Aspergillus) uncommon but severe (often prosthetic or immunocompromised).
- Culture-negative IE: prior antibiotics, fastidious agents (Coxiella burnetii, Bartonella, Tropheryma whipplei, Brucella, Legionella, fungi) or noninfectious mimics.
Clinical Manifestations
- Constitutional: fever (may be low-grade), chills, malaise, weight loss.
- Cardiac: new or changing murmur, heart failure (valve destruction, regurgitation, fistula), conduction abnormalities (perivalvular abscess).
- Embolic phenomena: stroke/TIA, splenic infarcts, renal infarcts, pulmonary septic emboli (right-sided), limb ischemia.
- Cutaneous/vascular: petechiae, splinter hemorrhages, Janeway lesions (painless palms/soles macules), Osler nodes (tender pulp nodules), Roth spots (retina).
- Immunologic: glomerulonephritis (hematuria/proteinuria), positive rheumatoid factor, immune complex vasculitis.
Diagnostic Approach
High suspicion in persistent bacteremia, fever with embolic events, new regurgitant murmur, or risk factors.
Blood Cultures
- Obtain ≥3 sets (aerobic + anaerobic bottles) from separate venipuncture sites over first 30–90 minutes before antibiotics if stable.
- Early empiric therapy warranted only after cultures drawn (unless shock/sepsis).
- Persistent bacteremia after 48–72 h of appropriate therapy prompts evaluation for uncontrolled source or resistant organism.
Echocardiography
- Transthoracic echo (TTE): first-line; sensitivity lower for prosthetic valves, obesity, small vegetations.
- Transesophageal echo (TEE): higher sensitivity for vegetations, abscesses, prosthetic involvement; indicated if TTE negative but suspicion high, prosthetic valves, intracardiac devices, S. aureus bacteremia, or complications suspected.
- Repeat imaging if clinical change (emboli, heart failure) or initial negative but suspicion persists.
Modified Duke Criteria (Summary)
Major criteria:
1. Positive blood cultures with typical IE organisms (e.g., ≥2 separate cultures of viridans streptococci, S. aureus, enterococci without primary focus; persistent positivity; single Coxiella burnetii positive or phase I IgG ≥1:800).
2. Evidence of endocardial involvement (echo: vegetation, abscess, new partial dehiscence of prosthetic valve; new valvular regurgitation).
Minor criteria:
– Predisposing heart condition or IVDU.
– Fever ≥38°C.
– Vascular phenomena (emboli, Janeway lesions, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage).
– Immunologic phenomena (Osler nodes, Roth spots, glomerulonephritis, rheumatoid factor).
– Microbiological evidence not meeting major (e.g., single positive culture of typical organism) or serology for atypical organism.
Diagnosis (traditional): Definite (pathologic OR clinical combinations), Possible, or Rejected based on combinations (not exhaustively reproduced here—apply full guideline tables in practice).
Additional Studies
- Laboratory: CBC (mild anemia), elevated ESR/CRP, rheumatoid factor, urinalysis (microscopic hematuria/proteinuria), serum creatinine.
- CT/MRI: detect embolic infarcts, mycotic aneurysms, splenic abscess.
- PET/CT or cardiac CT: adjunct in prosthetic/device IE for perivalvular infection or metabolic activity (where available).
Empiric Antimicrobial Therapy (Principles)
Tailor to native vs. prosthetic valve, community vs. healthcare acquisition, local resistance patterns. ALWAYS adjust when pathogen and susceptibilities known.
Examples (illustrative, not a substitute for guidelines):
– Native valve, community, subacute presentation: cover viridans streptococci & enterococci (e.g., ampicillin + ceftriaxone) if risk factors; or ceftriaxone monotherapy if typical and low resistance risk.
– Suspected S. aureus (acute, high fever, IVDU): anti-staphylococcal agent (e.g., oxacillin/nafcillin; vancomycin if MRSA risk or severe beta-lactam allergy).
– Prosthetic valve early or healthcare-associated: broader coverage (e.g., vancomycin + gentamicin (brief) + cefepime or an anti-pseudomonal beta-lactam) pending cultures.
– Culture-negative after adequate sampling: consider coverage for fastidious organisms; obtain serologies (Coxiella, Bartonella) and escalate diagnostics.
Duration typically 4–6 weeks (count from first negative culture) depending on organism and valve/prosthetic status.
Targeted Therapy (Selected Examples)
- Viridans streptococci (penicillin-susceptible): penicillin G or ceftriaxone ± gentamicin (short course) in uncomplicated native IE.
- MSSA native: nafcillin/oxacillin or cefazolin (if non-anaphylactic penicillin allergy).
- MRSA: vancomycin or daptomycin (avoid daptomycin in left-sided if guidelines contraindicate alternative indications not satisfied—follow current recommendations).
- Enterococcus faecalis: ampicillin + ceftriaxone (synergy) or ampicillin + gentamicin (monitor renal function); vancomycin-based regimens if beta-lactam intolerance.
- Prosthetic valve MRSA or resistant organisms: often combination therapy plus consider surgery.
- Fungal (Candida): liposomal amphotericin B ± flucytosine; early surgery common.
Indications for Early Surgical Intervention
- Heart failure from valvular dysfunction (acute severe regurgitation).
- Uncontrolled infection (abscess, persistent bacteremia >5–7 days on appropriate therapy, enlarging vegetation, prosthetic dehiscence).
- Prevention of embolism: large mobile vegetations (e.g., >10 mm with prior embolus; >15 mm left-sided even without embolus) — individualized.
- Fungal or highly resistant organisms.
Complications
Heart failure, systemic emboli (stroke, splenic infarct), mycotic aneurysm rupture, perivalvular abscess, conduction disturbances (AV block), glomerulonephritis, metastatic infections (vertebral osteomyelitis), sepsis.
Follow-Up & Monitoring
- Serial blood cultures until clearance (typically every 24–48 h).
- Repeat echocardiography if clinical deterioration or lack of improvement.
- Monitor drug toxicities (renal function, drug levels for vancomycin, CBC for cytopenias).
- Post-therapy surveillance: renewed fever → evaluate for relapse vs. alternative source.
Prevention (Antibiotic Prophylaxis — Selected Indications)
For certain high-risk patients undergoing dental procedures manipulating gingival tissue or perforating oral mucosa:
– Prosthetic cardiac valves or prosthetic material for valve repair.
– Prior infective endocarditis.
– Certain unrepaired cyanotic congenital heart diseases, or repaired with residual defects.
– Cardiac transplant recipients with valvulopathy.
Prophylaxis not recommended for most other valvular or congenital conditions. Emphasize meticulous oral hygiene and regular dental care.
Key Takeaways
- Obtain multiple blood cultures before antibiotics; early TEE improves detection of complications.
- Modified Duke criteria guide diagnosis, but clinical judgment remains vital—especially for prosthetic and device-related infections.
- Rapid pathogen identification and susceptibility-driven therapy plus timely surgery in selected cases reduce mortality and embolic risk.
- Preventive dental care and targeted prophylaxis protect the highest-risk groups without overusing antibiotics.
Educational information only; management should follow up-to-date cardiology/infectious disease guidelines and individualized specialist consultation.