Heart Attack (Myocardial Infarction): Recognize and Respond Fast
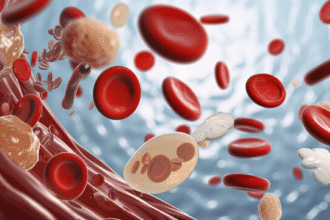
A heart attack (myocardial infarction, MI) happens when a coronary artery becomes blocked, cutting off blood flow to part of the heart muscle. The longer the blockage lasts, the more heart muscle is lost—fast action saves heart muscle and lives.
Common and Atypical Symptoms
Typical symptoms can start suddenly and last more than 10–30 minutes, not fully relieved by rest:
– Chest pressure, tightness, squeezing, burning, or pain
– Pain or discomfort radiating to the left or right arm, shoulder, neck, jaw, or upper back/epigastrium
– Shortness of breath
– Cold sweat, clammy skin
– Nausea or vomiting, lightheadedness, fainting
Atypical presentations are more common in older adults, people assigned female at birth, and those with diabetes:
– Unusual fatigue, weakness, or anxiety
– Shortness of breath without chest pain
– Indigestion-like discomfort, upper abdominal pain
Call emergency services if symptoms suggest a heart attack—even if they improve and then return.
What To Do Immediately (First Aid)
- Call your local emergency number now. Do not drive yourself. EMS can begin care and route you to a PCI-capable hospital.
- Rest in a comfortable position. Loosen tight clothing; avoid physical exertion.
- Chew aspirin if not allergic and not told to avoid it: 160–325 mg (1–2 regular tablets), chew and swallow. Do this only after calling EMS. Skip aspirin if you have a serious bleeding risk, allergy, or took a full dose very recently.
- Use prescribed nitroglycerin if you have it. Take as directed while seated; do not use someone else’s medication.
- If unresponsive and not breathing normally, start CPR and use an AED if available. Continue until help arrives.
What Not To Do
- Don’t wait to see if it passes; don’t drive yourself to the hospital.
- Don’t take non‑prescribed painkillers like NSAIDs (other than aspirin for MI) as they may worsen outcomes.
- Don’t eat or drink large amounts while awaiting EMS.
How Doctors Confirm a Heart Attack
Diagnosis combines:
– 12‑lead ECG: looks for ischemic changes (e.g., ST‑elevation/depression, new LBBB)
– Blood tests: cardiac troponins rise with heart muscle damage
– Clinical history and exam; imaging (echocardiography) when needed
Emergency Treatment Options (Hospital)
- Rapid antiplatelet therapy (aspirin; often plus a P2Y12 inhibitor)
- Reperfusion: primary PCI (angioplasty/stenting) is preferred when available quickly; otherwise, thrombolysis may be used for eligible STEMI patients
- Oxygen if hypoxemic, pain control, anticoagulation, and targeted management of rhythm or heart failure complications
Recovery and Secondary Prevention
After MI, long‑term treatments commonly include, as appropriate:
– Antiplatelet therapy (single or dual per cardiology guidance)
– High‑intensity statin
– Beta‑blocker; ACE inhibitor/ARB; SGLT2 inhibitor or MRA in selected patients
– Cardiac rehabilitation, physical activity plan, blood pressure/diabetes control
– Smoking cessation, healthy diet, weight and stress management
Risk Factors You Can Improve
- High blood pressure, high LDL cholesterol, diabetes
- Smoking, sedentary lifestyle, obesity
- Diet high in salt, saturated fat, and trans fat
- Chronic stress, sleep apnea
- Family history and age are non‑modifiable but still inform your risk
Note: This guide is for general education and does not replace professional medical care. Always follow local protocols and the advice of emergency and healthcare professionals.