Future Outlook for Liver Cancer Management with Emphasis on Neuroendocrine Liver Metastases (NELM)
Abstract
Liver involvement remains a pivotal determinant of prognosis in patients with neuroendocrine tumors (NETs). While immunotherapy has transformed outcomes in several malignancies, its role in NETs—particularly in neuroendocrine liver metastases (NELM)—remains exploratory with modest response rates. Progress in multidisciplinary coordination, optimal sequencing of locoregional and systemic therapies, biomarker-driven selection, and development of neoadjuvant strategies will define the next decade of care. This review synthesizes current practice patterns, limitations, and future directions.
- Abstract
- Scope and Definitions
- Current Treatment Landscape Overview
- Surgical Management
- Liver-Directed Locoregional Therapies
- Systemic Therapies
- Immunotherapy Status and Outlook
- Biomarker-Driven Selection
- Neoadjuvant and Adjuvant Considerations
- Multidisciplinary Coordination
- Research Gaps
- Practical Decision Framework (Simplified)
- Key Takeaways
- Future Directions
Scope and Definitions
| Term | Definition |
|——|————|
| NET | Well or moderately differentiated neuroendocrine tumor (G1–G2; some G3 differentiation now recognized) |
| NELM | Neuroendocrine liver metastases arising from primary NET (often small bowel, pancreas, lung) |
| Cytoreductive (Debulking) Surgery | Non‑curative resection aiming for predefined tumor burden reduction (≥70–80%) |
| Downstaging | Treatment strategy to convert unresectable to resectable disease |
Current Treatment Landscape Overview
| Modality | Typical Role | Strengths | Limitations |
|———-|————–|———–|————-|
| Surgical resection | Potentially curative or major cytoreduction | Survival benefit; symptom control | Not feasible in diffuse bilobar disease |
| Ablation (RFA/MWA) | Adjunct or for limited lesions | Organ-sparing; repeatable | Size/number constraints |
| Transarterial therapies (TAE/TACE/TARE) | Liver-dominant, unresectable disease | Tumor control, symptom relief | Post-embolization syndrome; heterogeneity of response |
| Systemic somatostatin analogs (SSAs) | First-line for functional & antiproliferative benefit | Low toxicity; symptom control | Modest tumor regression |
| PRRT (e.g., 177Lu-DOTATATE) | Progressive SSTR-positive disease | Durable control in selected patients | Requires adequate uptake & renal/bone marrow reserve |
| Targeted therapy (e.g., everolimus, sunitinib) | Progressive advanced pancreatic or other NET subtypes | Oral; PFS benefit | Cytopenias, stomatitis, metabolic effects |
| Chemotherapy | High-grade, pancreatic, or refractory disease | Higher response in selected subtypes | Toxicity; limited in indolent tumors |
| Immunotherapy (PD‑1/PD‑L1 ± CTLA‑4) | Biomarker-selected salvage (MSI-H, dMMR, TMB-H) | Durable responses in small biomarker subsets | Low ORR in unselected NETs |
| Liver transplantation | Highly selected unresectable NELM | Potential long-term survival | Scarce resource; strict criteria |
Surgical Management
Surgical resection remains the cornerstone where feasible. Goals include:
– Curative resection of primary + hepatic disease when R0/R1 achievable.
– Cytoreduction when ≥80–90% of intrahepatic tumor burden can be removed/ablated, improving hormonal symptom control and possibly survival.
– Integration with ablation to extend resection candidacy.
Patient Selection Considerations
- Performance status; hepatic reserve.
- Tumor distribution: unilobar vs diffuse bilobar.
- Extrahepatic disease: limited, indolent metastases may not preclude surgery.
- Ki-67 index and growth velocity.
Liver-Directed Locoregional Therapies
| Technique | Best Use Case | Key Notes |
|———-|—————|———–|
| RFA/MWA | ≤3–5 lesions, each <3–4 cm | Can be combined with limited resection |
| TAE/TACE | Hypervascular, liver-dominant progression | Symptom palliation (carcinoid syndrome) |
| TARE (Y-90) | Bilobar disease, prior therapy failure | Lower post-embolization syndrome; delayed response |
| Stereotactic Body Radiotherapy (SBRT) | Oligometastatic lesions unsuitable for ablation | Organ-sparing, dose constraints critical |
Systemic Therapies
- Somatostatin analogs (octreotide LAR, lanreotide): Disease stabilization and hormone control.
- PRRT: High uptake on somatostatin receptor imaging; emerging earlier-line positioning.
- Targeted agents: mTOR (everolimus) and multi-kinase inhibition (sunitinib) especially in pancreatic NETs.
- Chemotherapy: Temozolomide-based regimens (e.g., CAPTEM) in pancreatic NET; platinum-based in higher-grade or poorly differentiated NEC (distinct entity).
- Novel combinations under investigation (PRRT + radiosensitizers, targeted + immunotherapy).
Immunotherapy Status and Outlook
- Current Role: NOT standard for typical well-differentiated NETs; considered after multiple prior lines in biomarker-enriched subsets (MSI-H, dMMR, TMB-H).
- Rationale for Limited Activity: Low tumor mutational burden, immunologically “cold” microenvironment, stromal restriction.
- Investigational Strategies:
- Combination checkpoint blockade (PD‑1 + CTLA‑4) in higher grade subsets.
- Vascular normalization or stroma modulation preceding ICI.
- Peptide vaccines + checkpoint blockade.
- Adoptive cellular therapies (TIL, CAR-T) targeting NET antigens (under early exploration).
Biomarker-Driven Selection
| Biomarker | Implication | Testing Modality |
|———–|————|——————|
| MSI-H / dMMR | Consider PD‑1 inhibitor | IHC panel ± PCR/NGS |
| TMB-H | Potential ICI benefit | Comprehensive genomic profiling |
| SSTR expression | Eligibility for PRRT; SSA efficacy | 68Ga/64Cu-DOTATATE PET/CT |
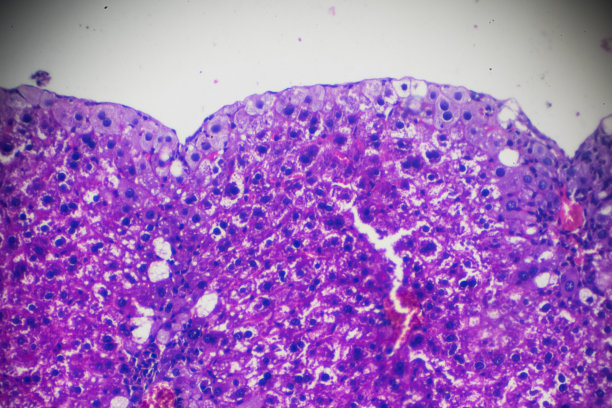
| Ki-67 index | Prognostic; guides intensity | Pathology (IHC) |
| Liver tumor burden % | Cytoreduction benefit threshold | Cross-sectional imaging |
Neoadjuvant and Adjuvant Considerations
- Evidence Gap: Few prospective trials assessing neoadjuvant strategies to downstage NELM.
- Potential Neoadjuvant Modalities: PRRT for volume reduction; targeted agents in pancreatic NET; selective arterial therapies.
- Adjuvant Therapy: No established standard after resection; individualized based on grade, margin status, residual disease.
Multidisciplinary Coordination
Integrated decision-making among hepatobiliary surgery, medical oncology, nuclear medicine, interventional radiology, pathology, and endocrinology optimizes sequencing. Regular tumor board review recommended at key junctures: initial diagnosis with liver involvement, pre-surgery, post-progression, and prior to transplant consideration.
Research Gaps
| Domain | Unmet Need |
|——–|———–|
| Immunotherapy | Strategies to convert “cold” NET microenvironment to inflamed phenotype |
| Neoadjuvant therapy | Prospective validation of downstaging algorithms |
| Sequencing | Optimal order: PRRT vs targeted vs liver-directed |
| Biomarkers | Predictors of PRRT response beyond SSTR intensity |
| Real-world outcomes | Standardized reporting of cytoreductive thresholds and survival |
Practical Decision Framework (Simplified)
- Confirm pathology + grade + Ki-67; stage with cross-sectional imaging + SSTR PET.
- Assess resectability (primary + liver). If resectable: plan combined surgery ± ablation.
- If unresectable but liver-dominant: evaluate for PRRT vs transarterial therapy vs systemic targeted agents.
- Biomarker testing (MSI/dMMR, TMB) in refractory disease before considering ICI.
- Re-evaluate for surgery after effective tumor downsizing.
- Manage recurrence with previously unused modality; maintain longitudinal multidisciplinary review.
Key Takeaways
- Surgery remains the only potentially curative modality; cytoreductive surgery can be justified when ≥80% debulking achievable.
- Locoregional therapies and PRRT are central in unresectable, liver-dominant disease.
- Immunotherapy currently has a niche role limited to biomarker-selected cases (MSI-H/dMMR, TMB-H); broad unselected use is not supported.
- Lack of robust neoadjuvant/adjuvant data presents an opportunity for prospective trials.
- Multidisciplinary, iterative reassessment is critical to capture windows for resection or transplant.
Future Directions
- Integration of radiomics and liquid biopsy (cfDNA, NET-specific markers) to guide dynamic treatment adjustment.
- Combination stromal remodeling + immunotherapy to enhance immune infiltration.
- Earlier-line PRRT sequencing studies and adaptive dosing models.
- Expanded transplant criteria using refined prognostic scoring.
Disclaimer: Educational synthesis for clinical context; not a substitute for individual patient management decisions.