Communicable Diseases: How Infections Spread and How to Stop Them
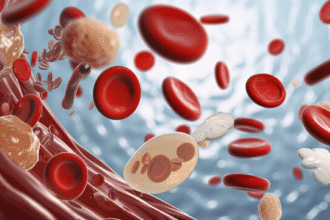
Communicable (infectious) diseases are caused by pathogens—bacteria, viruses, fungi, protozoa, or parasites—that move from one host to another. Infection means a pathogen enters and multiplies in the body; disease means that infection causes symptoms. People can carry and transmit pathogens even without symptoms (asymptomatic carriers).
How Transmission Happens
- Respiratory: droplets and aerosols from coughing, sneezing, talking, singing (e.g., influenza, COVID‑19, measles)
- Direct contact: skin/mucosal contact with lesions or secretions (e.g., HSV, varicella)
- Indirect contact (fomites): contaminated hands, surfaces, utensils
- Fecal–oral: contaminated food or water (e.g., cholera, norovirus, typhoid)
- Blood/body fluids: shared needles, needlesticks, transfusion, perinatal, or sexual exposure (e.g., HIV, hepatitis B/C)
- Vector‑borne: transmitted by mosquitoes, ticks, fleas (e.g., malaria, dengue, Lyme)
- Zoonotic: transmitted from animals (e.g., rabies, avian influenza)
Key concepts:
– Incubation period: time from exposure to symptoms
– Infectious period: time when a person can spread the pathogen (may begin before symptoms)
– Risk depends on dose/exposure, environment (ventilation, crowding), and host factors (age, immunity, comorbidities)
Breaking the Chain of Infection
- Vaccination: stay up to date on routine and risk‑based vaccines; boosters maintain protection and reduce spread
- Hand hygiene: wash with soap and water for ≥20 seconds or use alcohol rub (≥60% alcohol) when hands aren’t visibly soiled
- Respiratory etiquette and masks: cover coughs/sneezes; wear a well‑fitting mask in high‑risk settings or during outbreaks
- Ventilation and air cleaning: increase outdoor air, use HEPA filtration where feasible
- Safe food and water: cook thoroughly, avoid cross‑contamination, keep cold foods cold/hot foods hot; drink treated water
- Clean and disinfect high‑touch surfaces with appropriate products, especially when someone is ill
- Safer sex: use condoms; consider PrEP/PEP for HIV as advised by a clinician
- Needle safety: never share needles; use sterile equipment and harm‑reduction services where available
- Vector control: use repellents (e.g., DEET, picaridin), wear long sleeves, treat clothing/gear with permethrin, eliminate standing water
- Stay home when sick; isolate if contagious; follow testing and quarantine guidance after exposures
Care and Treatment Basics
- Antibiotics treat bacterial infections, not viral illnesses like colds or flu; avoid unnecessary antibiotics to prevent resistance
- Antivirals, antifungals, and antiparasitics are used for specific infections as prescribed
- Supportive care (rest, fluids, fever control) helps recovery; follow clinician advice
- Antimicrobial stewardship: take medications exactly as directed and complete prescribed courses
Vaccines and Immunity
- Active immunity: vaccines safely train the immune system to prevent severe disease and reduce transmission
- Passive immunity: antibodies (immunoglobulin) can provide short‑term protection after certain exposures
- Community protection (herd effects) improves as more people are immune, reducing spread to vulnerable individuals
When to Seek Medical Care Urgently
- Trouble breathing, chest pain, bluish lips/face, confusion, or severe drowsiness
- High fever that persists or any fever in infants under 3 months
- Signs of dehydration (very low urine, dizziness), persistent vomiting/diarrhea, or bloody stool
- Severe headache, stiff neck, rash with fever, or rapidly spreading skin infection
- If you are pregnant, very old/young, or immunocompromised and develop concerning symptoms
Everyday Prevention Checklist
- Wash hands regularly; avoid touching eyes, nose, and mouth with unwashed hands
- Keep vaccinations current for yourself and your household
- Improve indoor air (open windows when safe, use filtration)
- Practice safe food handling and drink safe water
- Use condoms and don’t share needles or personal items (razors, toothbrushes)
- Stay home when sick and test as recommended during outbreaks
This article is for general education and does not replace professional medical advice. Follow local public health guidance and consult a clinician for diagnosis and treatment.