A Healthy Lifestyle That Protects Your Kidneys
Protecting kidney function rests on a cluster of everyday habits that support fluid balance, metabolic waste clearance, vascular health, immune resilience, and appropriate nutrition. Small, consistent choices accumulated over months and years exert more influence than short bursts of intense effort. Understanding why each habit matters increases the likelihood of sustained adherence and early recognition of warning signs.
Hydration should be adequate but not excessive. The kidneys continuously regulate total body water and filter blood to excrete metabolic by‑products. Chronically low fluid intake or habitual urine retention concentrates the urine and can raise the risk of urinary tract infections and certain types of kidney stones. For many healthy adults, roughly 1.5 liters of plain, safe, unsweetened water distributed through the day supports normal physiologic processes, though needs vary with climate, activity, diet composition, medications, pregnancy, and comorbid conditions. Beverages high in added sugars, caffeine, sodium, or phosphates—such as many soft drinks, energy drinks, and some sweetened fruit beverages—should not routinely replace water because they may contribute to metabolic disturbances, elevated caloric intake, or subtle kidney stress over time.
Eliminating tobacco exposure and moderating or avoiding alcohol are foundational. Smoking accelerates vascular injury, promotes oxidative stress, and aggravates hypertension—each an independent contributor to chronic kidney disease (CKD) progression. In people living with diabetes or high blood pressure, tobacco further amplifies glomerular damage risk. Excessive alcohol intake can disrupt uric acid metabolism, contribute to dehydration, elevate blood pressure, and worsen underlying metabolic disorders, occasionally precipitating acute kidney injury in susceptible individuals. If alcohol is consumed, limiting both frequency and quantity in accordance with medical guidance helps mitigate risk; individuals with established kidney disease, uncontrolled hypertension, or certain medications may be advised to abstain entirely.
Balanced nutrition reduces avoidable renal workload while preserving overall health. Excessive habitual protein intake can increase intraglomerular pressure and filtration load in susceptible individuals, while chronically high sodium intake exacerbates hypertension and fluid retention. For most healthy adults, a protein intake in the range of about 0.8–1.2 grams per kilogram of body weight per day supports tissue maintenance without undue burden; higher targets may be appropriate temporarily for those engaged in structured resistance training or recovering from catabolic illness, ideally under professional guidance. Limiting added salt so that total sodium aligns with recommendations (for many, keeping salt to no more than about 6 grams per day, roughly equivalent to 2.4 grams of sodium) supports blood pressure control. Emphasizing minimally processed foods, diverse plant fibers, adequate potassium (when not contraindicated), and healthy fats contributes to cardiometabolic stability that indirectly protects the kidneys. Individualized adjustments—for example in protein, potassium, phosphorus, or fluid—should be made in consultation with a qualified clinician or dietitian when CKD, nephrolithiasis risk, or other conditions are present.
Reducing infection risk safeguards renal health because systemic and localized infections can trigger inflammatory cascades or direct tissue injury. Upper respiratory, gastrointestinal, urinary tract, and certain skin infections each have potential to exacerbate or precipitate renal problems, particularly in immunocompromised or high‑risk individuals. Preventive measures include good hand hygiene, regular ventilation of indoor spaces, avoidance of unnecessary exposure to crowded environments during peak outbreaks, appropriate mask use in high‑risk settings, safe food handling, staying current with recommended vaccinations (such as influenza, pneumococcal, hepatitis B, and others as indicated), prompt management of fevers or dysuria, and maintaining adequate sleep and nutrition to support immune function. Early evaluation of urinary symptoms (burning, frequency, flank pain, fever) or systemic signs (persistent high fever, unexplained swelling, reduced urine output) allows timely intervention.
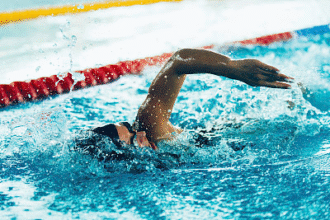
Attention to seemingly minor daily details—steady hydration, prudent dietary choices, avoidance of tobacco, moderated alcohol use, infection prevention, regular physical activity, weight management, adequate sleep, and periodic health screenings—creates a protective milieu for the kidneys. Individuals with risk factors such as diabetes, hypertension, autoimmune disease, recurrent stones, or a family history of kidney disease benefit from regular monitoring of blood pressure, estimated glomerular filtration rate (eGFR), urine albumin, and metabolic parameters. Taking a proactive, informed, and preventive stance helps preserve kidney function and overall vitality across the lifespan.