Evolution of Computed Tomography (CT): From First Generation to Photon-Counting Systems
1. Introduction
Computed Tomography (CT) transformed diagnostic imaging by enabling cross‑sectional visualization of internal anatomy with high geometric accuracy. Since Sir Godfrey Hounsfield’s prototype brain scanner (clinical debut 1972) and Allan Cormack’s mathematical groundwork (Radon transform application), CT technology has undergone rapid generational advancements improving speed, resolution, dose efficiency, and functional capabilities.
- 1. Introduction
- 2. Foundational Principles
- 3. Generational Hardware Evolution
- 4. Transition to Helical (Spiral) CT
- 5. Multi-Detector Array Impact
- 6. Temporal Resolution Strategies (Cardiac CT)
- 7. Dose Optimization Evolution
- 8. Spectral & Functional Advances
- 9. Reconstruction Method Progression
- 10. Common Artifacts & Mitigation
- 11. Clinical Impact by Domain
- 12. Photon-Counting CT: Next Frontier
- 13. Future Directions
- 14. Key Takeaways
2. Foundational Principles
| Concept | Description | Clinical Relevance |
|———|————-|——————–|
| X‑ray attenuation | Differential absorption measured along many projections | Basis for Hounsfield Unit (HU) mapping |
| Projection sampling | Multiple angular path integrals through voxel matrix | Adequate sampling prevents aliasing & artifacts |
| Reconstruction algorithms | Filtered back projection (FBP), iterative methods, model-based & AI-augmented | Dictate noise–resolution–dose trade-offs |
| Hounsfield Units | Normalized attenuation scale (water = 0 HU, air = −1000 HU) | Tissue characterization, lesion density metrics |
| Windowing | Level & width adjustments optimize contrast for tissue class | Brain vs lung vs mediastinum evaluation |
3. Generational Hardware Evolution
| Generation | Beam Geometry | Detector Configuration | Motion Pattern | Typical Scan Time (Single Slice) | Limitations |
|———–|—————|————————|—————|——————————|————-|
| 1st (1970s) | Pencil (narrow) | Single detector | Translate–rotate (1° steps) | 5–10 min / slice | Long time, motion artifacts |
| 2nd | Narrow fan | Multiple detectors (linear array) | Translate–rotate (10° steps) | 20–120 s / slice | Still slow; limited coverage |
| 3rd | Wide fan | Curved detector array (hundreds) | Rotate–rotate (tube + detectors) | 5–10 s / slice | Ring artifacts (detector calibration) |
| 4th | Wide fan | Stationary 360° detector ring | Rotate (tube only) | 2–5 s / slice | Cost, increased scatter |
| 5th (Electron Beam CT) | Electron beam + target rings | No mechanical rotation | Electronic sweeping | <100 ms (cardiac) | Limited adoption; spatial resolution constraints |
| Helical (Slip-ring era) | Continuous fan during table motion | Multi-row evolving | Spiral acquisition | Volume in single breath-hold | Initial interpolation artifacts |
| Multi-Detector CT (MDCT) | Broad fan / cone | 4 → 8 → 16 → 64 → 128 → 256+ rows | Continuous rotation (0.25–0.35 s) | Whole chest <5 s | Cone beam artifact management |
| Dual-Source | Two tubes/detector pairs | Orthogonal / offset geometry | Simultaneous rotations | Temporal res. ~66–75 ms | Increased complexity & dose planning |
| Photon-Counting CT | Narrower energy-resolving pixels | Semiconductor (CdTe/CdZnTe) | Standard rotation | Similar to MDCT (fast) | Technology cost; pile-up effects |
4. Transition to Helical (Spiral) CT
| Feature | Conventional Axial | Helical (Spiral) |
|———|——————-|——————|
| Table Motion | Step-and-shoot | Continuous |
| Data Coverage | Slice-by-slice | Continuous volumetric |
| Breath-Hold Demand | Multiple breath-holds | Single shorter breath-hold |
| Pitch (Definition) | N/A | Table travel per rotation / beam width |
| Advantages | High geometric fidelity | Faster, less misregistration, 3D reformats |
| Challenges | N/A | Interpolation & partial volume artifacts (mitigated by advanced reconstruction) |
5. Multi-Detector Array Impact
- Parallel acquisition of multiple slices increases z-axis coverage per rotation.
- Enables thin collimation (≤0.5–0.625 mm) → high-quality multiplanar & 3D reconstructions.
- Facilitates universal angiographic protocols (CTA for coronary, neurovascular, pulmonary, aortic).
- Reduces motion artifacts (rapid organ coverage).
6. Temporal Resolution Strategies (Cardiac CT)
| Approach | Mechanism | Benefit |
|———-|———-|———|
| Fast Gantry Rotation | 0.25–0.28 s rotation times | Improves single-segment temporal resolution |
| Dual-Source CT | Two tubes offset 90°–95° | Effective temporal resolution halves |
| Multi-segment Reconstruction | Combines data across cycles | Further resolution improvement; needs stable rhythm |
| Prospective ECG Triggering | Step-and-shoot phases | Dose reduction vs retrospective gating |
7. Dose Optimization Evolution
| Era | Dominant Technique | Dose Impact |
|—–|——————-|————-|
| Early FBP | Fixed mA, no modulation | Higher, non-optimized dose |
| Tube Current Modulation | Angular & z-axis modulation | 15–40% reduction |
| Automatic kV Selection | Patient-size adaptive | Improved contrast-to-noise + dose reduction |
| Iterative Reconstruction (ASIR, iDose, ADMIRE, VEO, MBIR) | Noise modeling & statistical optimization | 30–70% reduction (protocol dependent) |
| AI / Deep Learning Reconstruction | Neural noise suppression with texture preservation | Additional 20–40% potential reduction |
| Photon-Counting Spectral Optimization | Energy weighting, virtual monoenergetic images | Reduced contrast dose + improved CNR |
8. Spectral & Functional Advances
| Technology | Principle | Clinical Utility |
|———–|———-|——————|
| Dual-Energy (kVp switching, dual-layer, dual-source) | Two energy spectra differentiate materials | Gout crystal ID, renal stone typing, iodine mapping |
| Photon-Counting CT | Energy-resolved detection per photon | Improved spatial resolution, reduced electronic noise, multi-material decomposition |
| Perfusion CT | Dynamic time-resolved scans | Cerebral ischemia core vs penumbra; tumor perfusion |
| 4D CT | Temporal phases (e.g., airway, joint, perfusion) | Motion assessment, interventional planning |
9. Reconstruction Method Progression
| Method | Core Idea | Strengths | Limitations |
|——–|———-|———-|————|
| Filtered Back Projection (FBP) | Analytical inverse Radon transform with ramp filter | Fast, deterministic | Noise amplification at low dose |
| Hybrid Iterative | Combines FBP + iterative corrections | Balanced speed & noise reduction | Some smoothing artifacts |
| Model-Based Iterative (MBIR) | Detailed system + statistical modeling | Superior noise & artifact suppression | Computationally intensive |
| Deep Learning Reconstruction | Trained neural networks denoise / enhance | Texture preservation, speed | Data dependence, vendor variability |
10. Common Artifacts & Mitigation
| Artifact | Cause | Mitigation |
|———|——|———–|
| Beam Hardening | Polychromatic spectrum through dense object | Filtration, iterative correction, dual-energy |
| Partial Volume | Thick slices averaging densities | Use thin slices, overlapping reconstructions |
| Motion (respiratory, cardiac) | Patient or physiologic motion | Faster acquisition, gating, coaching |
| Ring Artifact | Detector calibration drift (3rd gen) | Calibration, detector replacement |
| Metal Streak | Photon starvation & beam hardening | MAR algorithms, dual-energy, higher kVp |
| Cone Beam | Wide z-cover causing interpolation errors | Advanced cone-beam reconstruction kernels |
11. Clinical Impact by Domain
| Domain | Transformative Applications |
|——–|—————————–|
| Neuroimaging | Acute stroke triage (NCCT, CTA, perfusion), hemorrhage detection |
| Cardiovascular | Coronary CTA, TAVR planning, aortic dissection evaluation |
| Oncology | Staging (chest/abdomen/pelvis), radiotherapy planning |
| Trauma | Whole-body polytrauma (pan-scan) rapid survey |
| Pulmonology | Lung nodule screening (LDCT), interstitial lung disease phenotyping |
| Musculoskeletal | Occult fractures, complex joint morphology |
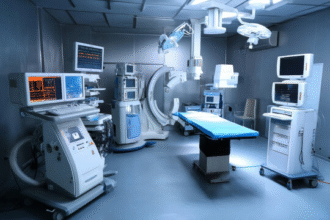
| Interventional | CT-guided biopsy, ablation planning, navigation |
12. Photon-Counting CT: Next Frontier
- Semiconductor detectors directly convert X‑ray photons to electrical signals, eliminating scintillation layer and reducing electronic noise.
- Energy discrimination enables virtual non-contrast images, quantitative iodine mapping, metal artifact reduction.
- Smaller detector pixels → higher intrinsic spatial resolution (benefits small vessel, bone microarchitecture, lung detail).
- Potential for reduced contrast media volume and radiation dose while enhancing lesion conspicuity.
13. Future Directions
| Innovation | Potential Benefit |
|———–|——————|
| AI Protocol Orchestration | Personalized kVp/mA & contrast timing per patient physiology |
| Integrated Radiomics Pipelines | Automated feature extraction for prognostication |
| Real-Time Motion Compensation | Improves cardiac & pulmonary imaging fidelity |
| Ultra-High Resolution Modes | Microvasculature & trabecular detail characterization |
| Multi-contrast (K-edge) Imaging | Targeted molecular / functional assessment |
14. Key Takeaways
- CT evolution progressed from slow translate–rotate single-slice systems to high-speed multi-detector, dual-source, and emerging photon-counting architectures.
- Advances in detector design, rotation mechanics, and reconstruction algorithms enabled drastic reductions in scan time and radiation dose while expanding clinical indications.
- Spectral and functional techniques provide material differentiation and physiologic insights beyond density alone.
- Photon-counting CT represents a paradigm shift with improved spatial resolution and spectral fidelity poised to refine oncologic, cardiovascular, and musculoskeletal imaging.
- Ongoing integration of AI and radiomics will further individualize protocols and enhance diagnostic & prognostic value.
Disclaimer: Educational overview; adhere to local radiation safety regulations and vendor-specific operational guidelines.