Hepatitis: A Practical, Evidence‑Based Guide
Hepatitis means inflammation and injury of the liver. It has many causes—viruses (A–E), alcohol, medications/toxins, autoimmune disease, metabolic/genetic conditions, and fatty liver disease. Severity ranges from mild, short‑lived illness to chronic disease with cirrhosis and liver cancer.
Hepatitis at a Glance
- Key symptoms: fatigue, loss of appetite, nausea, right‑upper‑quadrant discomfort, dark urine, pale stools, jaundice (yellowing of skin/eyes), itching
- Duration: acute (<6 months) vs. chronic (≥6 months)
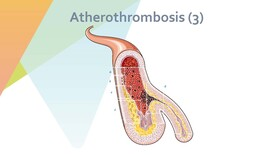
- Major complications: acute liver failure (rare), chronic hepatitis → fibrosis/cirrhosis, portal hypertension, hepatocellular carcinoma (HCC)
Types and Common Causes
Viral Hepatitis (A–E)
- Hepatitis A (HAV): fecal–oral transmission (contaminated food/water; travel/outbreaks). Acute disease only; most recover fully. Vaccine preventable.
- Hepatitis B (HBV): blood, sexual, and perinatal transmission. Can become chronic, especially if acquired at birth/early childhood. Vaccine preventable.
- Hepatitis C (HCV): primarily blood‑borne (needles/medical exposures). Often becomes chronic without treatment; now curable with direct‑acting antivirals (DAAs).
- Hepatitis D (HDV): defective virus requiring HBV coinfection; worsens HBV disease. Prevented indirectly by HBV vaccination.
- Hepatitis E (HEV): fecal–oral, often water‑borne; usually acute. Can be severe in pregnancy and chronic in the immunocompromised.
Non‑Viral Causes
- Alcohol‑related hepatitis: heavy alcohol use causing liver inflammation and steatohepatitis
- Drug‑induced liver injury (DILI): prescription/OTC/herbal supplements (e.g., high‑dose acetaminophen, some antibiotics, bodybuilding supplements)
- Nonalcoholic fatty liver disease (NAFLD/NASH): fat accumulation and inflammation linked to obesity, insulin resistance, and dyslipidemia
- Autoimmune hepatitis: immune‑mediated liver attack; often responsive to immunosuppression
- Genetic/metabolic and toxins: hemochromatosis (iron overload), Wilson disease (copper), alpha‑1 antitrypsin deficiency; industrial or environmental toxins
Symptoms and When to Seek Care
- Common symptoms: fatigue, anorexia, nausea/vomiting, abdominal fullness/bloating, right‑upper‑quadrant pain, dark urine, pale/clay‑colored stools, jaundice, itching
- Seek urgent care for: confusion/sleepiness (possible encephalopathy), severe abdominal swelling, vomiting blood or black stools, intense jaundice with very dark urine, easy bruising/bleeding, severe weakness—these can signal liver failure or portal hypertension
How Hepatitis Affects Metabolism and Nutrition
Liver injury disrupts multiple metabolic pathways:
– Carbohydrates: reduced glycogen synthesis and impaired lactate clearance can predispose to low blood sugar and lactic acid buildup (aches, fatigue)
– Proteins: decreased albumin lowers oncotic pressure (edema/ascites); reduced clotting‑factor synthesis raises bleeding risk; impaired urea cycle can increase blood ammonia
– Lipids: impaired export of triglycerides leads to fat accumulation (fatty liver) and, over time, scarring (fibrosis/cirrhosis)
– Vitamins/minerals: disrupted storage/activation of fat‑soluble vitamins (A, D, E, K) and many B vitamins; altered handling of iron and copper
Practical nutrition notes:
– Adequate calories and protein are important—even in chronic disease—unless a clinician advises temporary restriction during severe encephalopathy
– Small, frequent meals; include a bedtime snack (helps prevent overnight catabolism)
– Sodium restriction for ascites/edema; limit highly processed foods
– Alcohol abstinence is critical in alcohol‑related and most chronic liver diseases
– Consider supervised vitamin/mineral repletion when deficient (e.g., thiamine in alcohol use disorder; fat‑soluble vitamins in cholestasis)
Diagnosis
- Blood tests: AST/ALT, alkaline phosphatase, GGT, bilirubin, albumin, INR, platelet count
- Viral serology/virology: HAV IgM; HBsAg, anti‑HBc, HBeAg, HBV DNA; HCV antibody and HCV RNA; HEV testing in select cases
- Autoimmune markers (ANA, SMA, IgG), iron studies, ceruloplasmin, alpha‑1 antitrypsin phenotype when indicated
- Imaging: abdominal ultrasound; elastography (FibroScan) to assess fibrosis; CT/MRI in select cases
- Liver biopsy: when diagnosis or stage remains uncertain
Treatment Overview (Cause‑Specific)
- HAV/HEV: supportive care (hydration, rest, anti‑nausea meds). Most recover fully. HEV in pregnancy or immunocompromised needs specialist care.
- HBV: long‑term suppression with potent nucleos(t)ide analogs (tenofovir DF/AF, entecavir); pegylated interferon in selected patients. Regular monitoring to assess activity and fibrosis.
- HCV: short courses (8–12 weeks) of oral DAAs (e.g., sofosbuvir/velpatasvir or glecaprevir/pibrentasvir) cure >95% of patients.
- Alcohol‑related hepatitis: strict abstinence, nutrition support; corticosteroids in selected severe cases after exclusion of infection and GI bleeding; treat complications of cirrhosis.
- Autoimmune hepatitis: corticosteroids ± azathioprine (or other immunosuppressants) under specialist supervision.
- DILI: stop the offending agent; supportive care; N‑acetylcysteine for acetaminophen toxicity.
- NAFLD/NASH: weight reduction (target 7–10% loss), regular exercise, optimize diabetes/lipids/blood pressure; consider pharmacotherapy per guidelines.
Monitoring and Complications
- Fibrosis assessment over time (elastography/biomarkers)
- Cirrhosis management: screen and manage varices, ascites, encephalopathy, infections
- HCC surveillance: ultrasound ± alpha‑fetoprotein every 6 months for all with cirrhosis and for certain HBV patients even without cirrhosis (per guidelines)
Prevention
- Vaccination: HAV and HBV vaccines are highly effective; vaccinate at‑risk adults and all children. No vaccine for HCV/HDV/HEV in many regions.
- Reduce transmission: safe sex (condoms), don’t share needles or personal items (razors/toothbrushes), ensure sterile medical/dental equipment, screen blood products
- Food and water safety: especially important for HAV/HEV and travel to endemic regions
- Alcohol moderation/abstinence; avoid unnecessary hepatotoxic drugs/supplements; discuss new supplements/medications with a clinician
This article is for general education and does not replace professional medical advice. For diagnosis, treatment choices, vaccinations, and nutrition plans tailored to you, consult a qualified healthcare professional and follow local clinical guidance.